SINGAPORE – Cancer tumours that were surgically removed from patients can now be kept alive for the next 10 days so that different anti-cancer drugs and treatments can be tested on them.
This will save cancer patients from receiving unnecessary and expensive treatments, or wasting time on therapies that prove to be ineffective.
Singapore scientists bioengineered a jelly-like hydrogel based on hyaluronic acid, a water-retentive substance found naturally in human tissues and fluids in the skin, joints and eyes.
This hydrogel can significantly extend the viability of tumour fragments’ composition and “architecture”, where such cultures would otherwise disintegrate after no more than a few hours to one to two days outside the body.
Drug testing and the studying of molecular and cellular processes typically require longer culture durations.
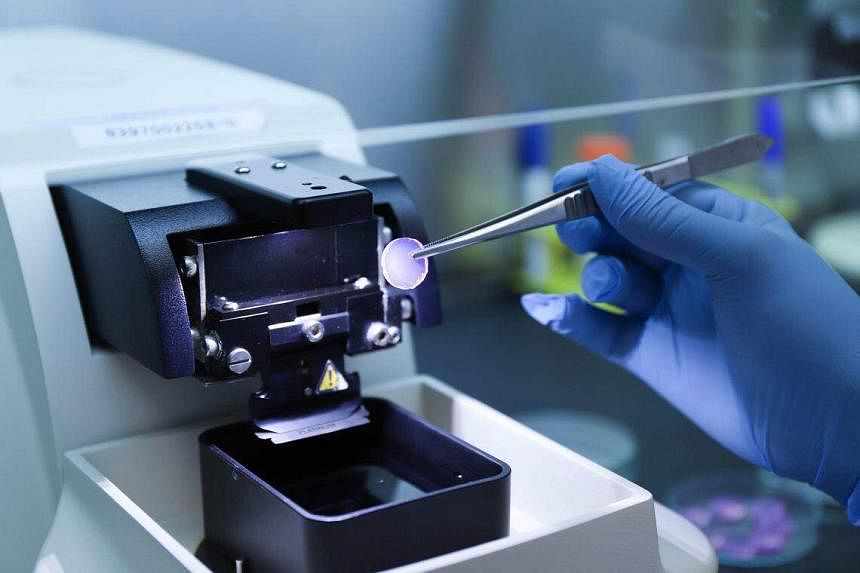
The researchers used a vibrating microtome machine to shave precise fragments of the tumour removed from the patient, to be cultivated on a hydrogel disc.
“We used the hydrogel to culture fragments of tumours taken from the squamous cells of patients with head and neck cancers, and found that it was promising in preserving them for the testing of drugs,” said Assistant Professor Eliza Fong, who co-authored the study.
“It also worked on different cancer types, such as peritoneal, lung, colorectal and ovarian,” added Prof Fong, who is from the department of biomedical engineering at the National University of Singapore College of Design and Engineering.
The results of the study were published in peer-reviewed journal Biomaterials on Jan 20.
Professor Gopal Iyer, a co-author of the study and head of the department of head and neck surgery at the National Cancer Centre Singapore, said cancer is the biggest bugbear when it comes to precision treatments.
“For years, I have been trying to remove tumour cells from patients and grow them to figure out whether they could inform me on how patients respond to anti-cancer drugs; but there is more to the tumour than mere cancer cells.
“Unfortunately – or fortunately – about five to 10 years ago, there was an explosion of immunotherapy. That blew my models out of the water,” he said.
Immunotherapy is a targeted approach that involves boosting the body’s immune system to recognise, target and destroy cancer cells.
Tumours are highly complex tissues comprising not only the rapidly proliferating cancer cells, but also an array of supporting cells such as immune cells.
This means that two patients with the same type of cancer may respond differently to the same drug.
Because the hydrogel preserves the whole tumour, scientists will be able to test not only anti-cancer drugs but also immunotherapies.
Prof Fong likened the preserved fragments to “true patient avatars for personalised and precision oncology”.

Professor Lee Soo Chin, who heads the department of haematology-oncology at the National University Cancer Institute, Singapore (NCIS), said the method can potentially be used to guide treatment selection in a real-time fashion for individual patients.
The drug chosen after testing the preserved tumour cells would then be evaluated for its efficacy when used on the actual patient.
Prof Lee, who was not involved in the study, said patient outcomes would improve if this method is proven to be able to accurately select the best drug for the patient.
She said that currently in the clinic, selection of cancer drug for the individual patient is still based on physician experience and published literature on patient populations, and not usually individualised for each patient.
“This new method can potentially cut down on treatment cost in general, as there will be fewer ‘misses’,” she added.
Prof Lee cited a 2021 NCIS trial on six patients with advanced gastric cancer, where drugs were tested on cancer cells from patients extracted during their biopsy to see if they would be effective, prior to putting patients through treatment.
Its aim was to save patients with advanced cancers from receiving unnecessary treatments.
Prof Fong noted that the NCIS study tested drugs on only cancer cells, but “many drugs now target the supporting cells to eliminate cancer cells”.
The new hydrogel allows various drugs to be tested for efficacy against both cancer cells and the supporting cells of a tumour.
“This opens up unprecedented opportunities for the effective and accurate testing of anti-cancer drugs and immunotherapies on the tumour,” Prof Fong said.

Cancer survivor Or Yan Nee, 53, suffered nausea, dizziness, fatigue and constipation as side effects of chemotherapy after she was diagnosed with oropharyngeal cancer in May 2023.
This cancer affects the back of the throat, base of the tongue and tonsils. She went through three rounds of chemotherapy and 33 rounds of proton therapy.
“I also had some ulcers in the mouth, redness on my neck and temporary loss of my sense of taste after proton therapy,” said the part-time infant care teacher assistant.
Had the new hydrogel technology been developed earlier, it might have saved her from her sufferings.
“If this new hydrogel technology can help doctors to find out what treatment suits patients and help cure them, I think that’s great,” Ms Or said.
Prof Iyer said curing cancer was mostly a distant goal – but this breakthrough in personalised precision treatment will increase the chances of managing cancer like a chronic disease in the future.
“Curing cancer is a nice cliche. With humans living longer, the aim is to treat cancer as a chronic disease and manage it. That is a more realistic objective,” he said.


